Abstract
Background Non-first-degree (NFD) related donors can be considered as alternatives for first-degree (FD) related donors in haploidentical hematopoietic cell transplantation (haplo-HCT), but the efficacy of these transplants remains uncertain. We therefore compared the outcomes of NFD and FD related haplo-HCTs for acute leukemia patients in complete remission (CR).
Patients and Methods We retrospectively analyzed 2703 acute myeloid leukemia (AML: n=2047) and acute lymphoblastic leukemia (ALL: n=656) patients in CR who received a haplo-HCT from 2010-2021 in 177 EBMT centers participating in the study. Exact matching and propensity score (PS) matching was used for pair-matching. The following variables were used for exact matching: diagnosis, status at transplant, patient age per 5 years, GVHD prophylaxis. The propensity score was based on patient sex and conditioning intensity. The NFD-to-FD ratio was 1:3, but patients with only 1 or 2 controls were included in the analysis.
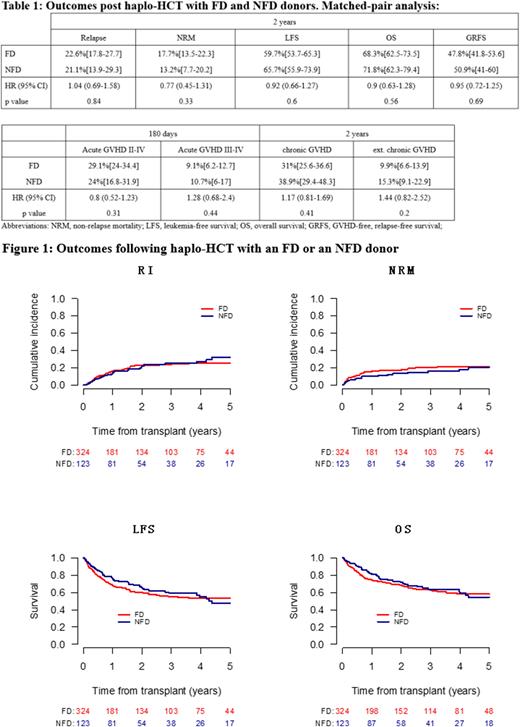
Results One hundred and twenty-three NFD were matched with 324 FD. The patients were well matched with standardized mean difference estimates of less than 5% for all matched parameters. .
Myeloablative conditioning was used in 65% and 69% of FD and NFD patients, respectively. The source of stem cells was peripheral blood (PB) alone in 46% and 68%, respectively. Both cohorts reached good engraftment rates (FD: 95.6% vs. NFD: 96.7%, p= 0.78). The 180-day cumulative incidence (CI) of grade II-IV acute graft-versus-host disease (GVHD) (FD: 29.1% vs. NFD: 24%, p= 0.31), and the 2-year CI of extensive chronic GVHD (FD: 9.9% vs. NFD: 15.3%, p= 0.2) were comparable between the two cohorts. No differences were observed between the two cohorts in 2-year CIs of relapse (FD: 22.6% vs. NFD: 22.1%, p=0.84) and non-relapse mortality (NRM) (FD: 17.7% vs. NFD: 13.2%, p=0.33). The 2-year probabilities of overall survival (OS) (FD: 68.3% vs. NFD: 71.8%, p=0.56), leukemia-free survival (LFS) (FD: 59.7% vs. NFD: 65.7%, p=0.6), and GVHD-free, relapse-free survival (GRFS) (FD: 47.8% vs. NFD: 50.9%, p=0.69) were similar between the two cohorts (Table 1 and Figure 1). The three major causes of death in FD and NFD were relapse (41% and 46%), GVHD (13% and 29%), and infection (30% and 15%), respectively.
Conclusion No significant differences were observed in outcomes following haplo-HCT using NFD or FD donors in this retrospective matched-pair analysis. Our findings support the consideration of NFD donors for haplo-HCT when there is no available FD donor. If both donor types are available, an additional question may be to identify other important factors such as donor age and cytomegalovirus (CMV) status where the NFD donor might be a better choice than a FD donor.
Disclosures
Labopin:Jazz Pharmaceuticals: Honoraria. Ciceri:Kite Pharma: Consultancy. Mohty:Celgene: Honoraria; Bristol Myers Squibb: Honoraria; Takeda: Honoraria; Amgen: Honoraria; Novartis: Honoraria; Adaptive Biotechnologies: Honoraria; Astellas: Honoraria; Oncopeptides: Honoraria; Pfizer,: Honoraria; GSK: Honoraria; Jazz Pharmaceuticals: Honoraria, Research Funding; Sanofi: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Gilead: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal